Overview of Panic Disorder
Panic disorder is a type of anxiety disorder characterized by sudden, unexpected, and intense episodes of panic, known as panic attacks. These attacks can occur without any clear trigger, often leaving the individual with overwhelming feelings of fear and physical symptoms like a racing heart, shortness of breath, dizziness, or a sense of losing control. In India, where mental health is still often stigmatized or misunderstood, individuals with panic disorder may struggle to get timely and appropriate treatment, compounding the problem.
Panic disorder can severely disrupt a person’s life, interfering with daily activities, work, and relationships. However, with increased awareness and access to mental health care, people can manage this condition effectively. This article explores the causes, symptoms, and treatment options for panic disorder in the context of the Indian population.
Panic disorder is a debilitating condition that causes sudden and repeated episodes of intense fear, which are often accompanied by physical symptoms such as chest pain, heart palpitations, dizziness, and shortness of breath. These episodes, known as panic attacks, can occur unexpectedly, without any identifiable cause or trigger. Many individuals with panic disorder live in constant fear of experiencing another attack, which can lead to agoraphobia, a condition where they avoid places or situations where they might feel trapped or helpless during an attack.
In India, panic disorder is not always well-understood, and individuals experiencing symptoms may be misdiagnosed with other physical ailments or may hesitate to seek help due to the stigma surrounding mental health. However, with increasing awareness and access to mental health services, more people are beginning to recognize and address the disorder.
Key Facts
- Panic disorder is an anxiety disorder marked by recurrent panic attacks, often occurring unexpectedly.
- Around 2-3% of people worldwide suffer from panic disorder, and similar prevalence rates are expected in India.
- Panic disorder often develops in early adulthood but can affect people of all ages.
- With proper treatment, such as therapy and medication, most individuals with panic disorder can lead normal, productive lives.
Symptoms of Panic Disorder
Panic attacks are the hallmark symptom of panic disorder. These attacks can occur without warning and typically peak within 10 minutes, though their effects can last much longer.
- Physical Symptoms:
- Panic disorder or a racing heart
- Shortness of breath or hyperventilation
- Chest pain or discomfort
- Sweating, trembling, or shaking
- Dizziness or feeling lightheaded
- Nausea or stomach upset
- Hot flashes or chills
- Numbness or tingling in the hands or feet
- Emotional and Cognitive Symptoms:
- Intense fear or anxiety, sometimes described as a sense of impending doom or death
- Feeling detached from reality, known as derealization, or feeling detached from oneself, called depersonalization
- A feeling of losing control or going crazy
- Constant worry about having more attacks
- Behavioral Symptoms:
- Avoidance of places or situations that might trigger a panic attack or where help may not be easily available (e.g., crowded places, public transportation)
- Social withdrawal due to the fear of being embarrassed or vulnerable during a panic attack
Risk Factors and Causes
Panic disorder is a complex condition, and a variety of factors can contribute to its development. In India, these factors may include genetic predisposition, environmental stressors, and cultural or societal pressures.
- Genetic Predisposition: Individuals with a family history of panic disorder or other anxiety disorders may be more likely to develop panic disorder themselves. The condition is thought to have a hereditary component, as studies suggest that panic disorder can run in families.
- Life Stressors: Significant life events, such as job loss, financial difficulties, family conflicts, or the death of a loved one, can trigger the onset of panic disorder. In India, societal expectations related to career, marriage, and family roles can contribute to chronic stress, which may precipitate panic attacks.
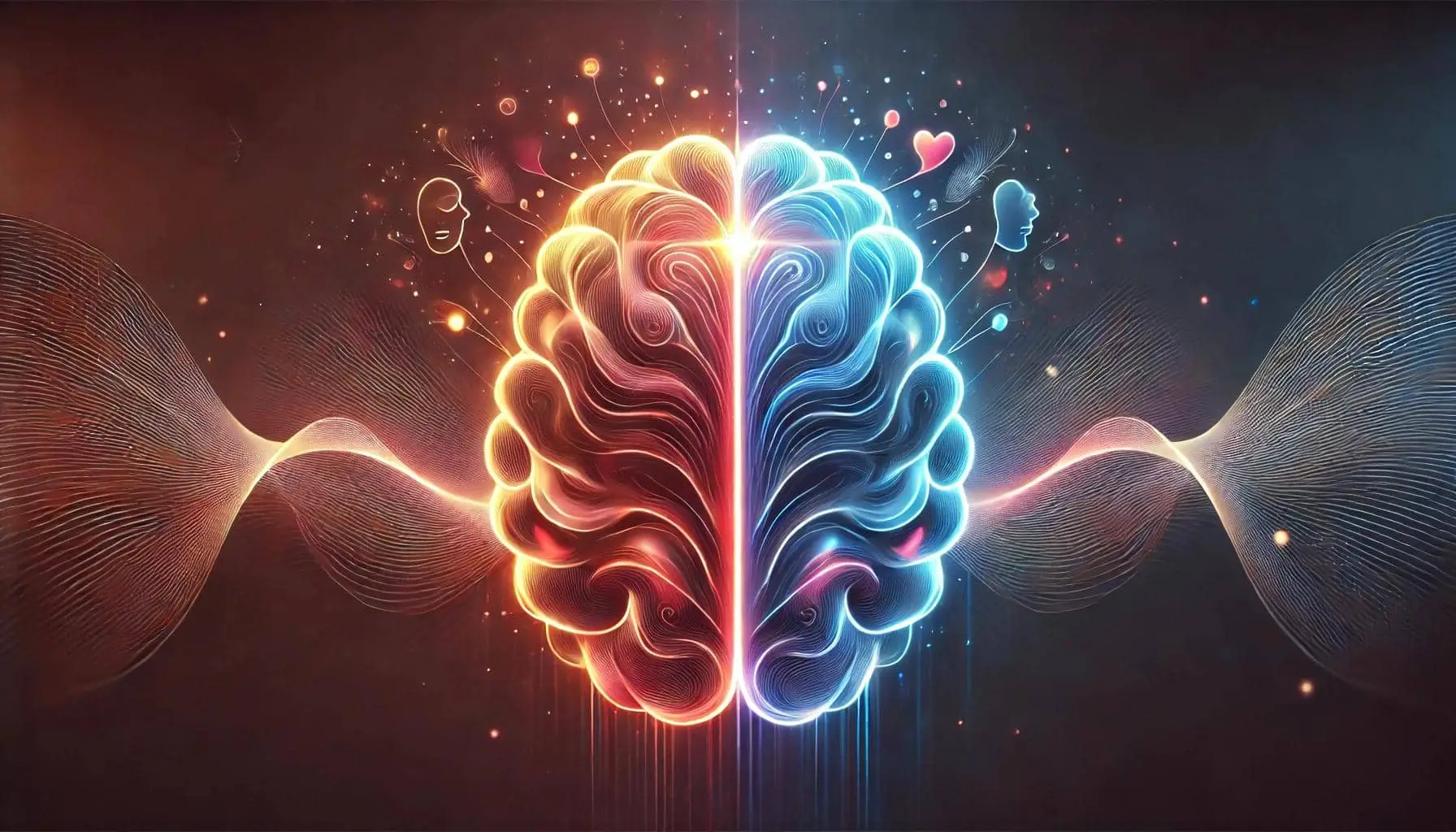
- Biological Factors: Imbalances in brain chemicals like serotonin and norepinephrine may play a role in panic disorder. Additionally, individuals with panic disorder may have an overactive fight-or-flight response, leading to the body reacting to perceived threats with heightened fear and physical symptoms.
- Cultural and Social Factors: In India, where mental health issues are sometimes viewed as a weakness or even spiritual affliction, individuals with panic disorder may experience additional stress from societal judgment or lack of understanding. The pressure to conform to social norms and succeed in competitive environments can exacerbate anxiety and contribute to panic disorder.
- Substance Use: Excessive use of caffeine, nicotine, or other stimulants, which are commonly consumed in India in the form of tea, coffee, and tobacco, can increase anxiety and trigger panic attacks.
Impact of Panic Disorder on Daily Life
Living with panic disorder can be deeply distressing. The unpredictability of panic attacks leads many individuals to develop anticipatory anxiety—the fear of having another attack. This can result in avoidance behavior, where individuals limit their activities, avoid social gatherings, or even become housebound. This isolation can lead to additional mental health issues such as depression.
In India, where close family ties and social interactions are integral to daily life, individuals with panic disorder may find it especially difficult to avoid social events, family obligations, or work responsibilities, exacerbating feelings of guilt, shame, or inadequacy.
Treatment and Care
Panic disorder is a treatable condition, and with the right approach, individuals can manage symptoms and lead fulfilling lives. Treatment usually involves a combination of psychotherapy, medication, and lifestyle adjustments.
- Cognitive Behavioral Therapy (CBT): CBT is one of the most effective therapies for panic disorder. It helps individuals understand the relationship between their thoughts, feelings, and behaviors. CBT for panic disorder often involves exposure therapy, where individuals are gradually exposed to their fears in a controlled environment, helping them learn how to manage their anxiety.
- Mindfulness and Relaxation Techniques: Practices such as mindfulness meditation, pranayama (breath control), and yoga—which are integral to Indian culture—can help individuals manage the physical and emotional symptoms of panic disorder. These practices teach individuals to stay present in the moment and reduce anticipatory anxiety.
- Medication:
- Antidepressants, particularly Selective Serotonin Reuptake Inhibitors (SSRIs), are often prescribed to help regulate mood and reduce anxiety.
- Benzodiazepines may be used on a short-term basis to control acute panic symptoms, but they are not recommended for long-term use due to the risk of dependence.
- Beta-blockers may help control the physical symptoms of panic attacks, such as rapid heart rate or trembling.
- Lifestyle Adjustments:
- Exercise: Regular physical activity can reduce anxiety and improve overall mental health. Activities like walking, swimming, or cycling are highly beneficial.
- Sleep Hygiene: Establishing a consistent sleep routine can help reduce anxiety levels and prevent panic attacks triggered by fatigue.
- Dietary Changes: Limiting caffeine and avoiding stimulants like nicotine can help reduce anxiety and the likelihood of panic attacks.
- Support Systems: Building a support network is crucial in managing panic disorder. In India, where family support is often central, involving close family members in therapy can help the individual feel understood and less isolated. Mental health support groups are also becoming more accessible, providing individuals with a safe space to share their experiences and gain support.
Coping Strategies
In addition to professional treatment, individuals with panic disorder can use coping strategies to manage their symptoms in daily life.
- Deep Breathing: During a panic attack, focusing on slow, deep breathing can help reduce symptoms like hyperventilation and dizziness. Practicing diaphragmatic breathing can bring the body back to a state of calm.
- Grounding Techniques: Techniques such as 5-4-3-2-1, which involve engaging the five senses to reconnect with the present moment, can help manage the sense of unreality or detachment often felt during a panic attack.
- Avoiding Negative Thought Patterns: Individuals can challenge catastrophic thoughts and reframe them into more realistic scenarios. For instance, instead of thinking, “I’m going to die,” they can replace it with, “This is just a panic attack. It will pass.”
- Seeking Help Early: Recognizing the symptoms of panic disorder early and seeking help can prevent the condition from worsening. In India, where people may hesitate to seek mental health care, increasing awareness and removing stigma is crucial.
Conclusion
Panic disorder is a serious but treatable condition that affects millions of people, including many in India. By understanding the symptoms, causes, and available treatments, individuals with panic disorder can take steps toward managing their condition and improving their quality of life. With increased awareness, accessible mental health services, and a supportive community, people with panic disorder in India can overcome the challenges they face and lead healthy, fulfilling lives. It is essential to break the stigma around mental health and encourage open conversations about conditions like panic disorder, ensuring that no one suffers in silence.